Vitamin D
- Helder Barroso

- Apr 23, 2019
- 5 min read
Vitamin D is a fat-soluble nutrient. It is one of the 24 micronutrients critical for human survival. The sun is the major natural source of the nutrient, but vitamin D is also found naturally in fish and eggs. It is also added to dairy products.
Supplemental vitamin D is associated with a wide range of benefits, including increased cognition, immune health, bone health and well-being. Supplementation can also reduce the risks of cancer, heart disease, diabetes and multiple sclerosis. People deficient in vitamin D may also experience increased testosterone levels after supplementation.
The body produces vitamin D from cholesterol, provided there is an adequate amount of UV light from sun exposure. There is only a sufficient amount of UV light coming from the sun when the UV index is 3 or higher, which only occurs year-round near the equator, between the 37th parallels.
Most people are not deficient in vitamin D, but they do not have an optimal level of vitamin D either. Due to the many health benefits of vitamin D, supplementation is encouraged if optimal levels are not present in the body.
Depression is associated with vitamin D insufficiency but it doesn’t mean that vitamin D insufficiency is the cause (or the only cause) of the depression. During the winter months, when there is less sun, we might suffer from seasonal affective disorder (SAD), which has been associated both with a decrease in vitamin D production (due to a decrease in exposure to the UVB spectrum of sun rays) and with a decrease in illumination (a decrease in exposure to the visible spectrum of sun rays).
Five successive reviews looked at the effects of supplemental vitamin D on mood. The 2015 review found no significant reduction in depression, though its authors didn’t rule out the possibility that supplemental vitamin D could be more effective in people with higher levels of depression or lower levels of vitamin D than seen in most studies. The four other reviews — published in 2014, 2016, 2017, and 2018 — found benefit from supplementation, but three mentioned low methodological quality, and two mentioned high risk of publication bias (of the other two, one found minimal bias and the other failed to account for bias).
In the UK, the Recommended Daily Allowance (RDA) for vitamin D falls between 400 and 800 IU (International Units). These amounts, which some researchers criticize as inadequate, can be obtained naturally from only a few foods sources, notably fatty fish (such as salmon, tuna, and sardines). However, milk is often fortified with vitamin D.

Since few foods are rich in vitamin D, supplementation is a valid option. Should your blood test show that your vitamin D levels are low, start supplementing with 2,000 IU/day (a number that, based on the available evidence, should provide the best balance of efficacy and safety), then get tested again after a couple of months.
Sources of Vitamin D
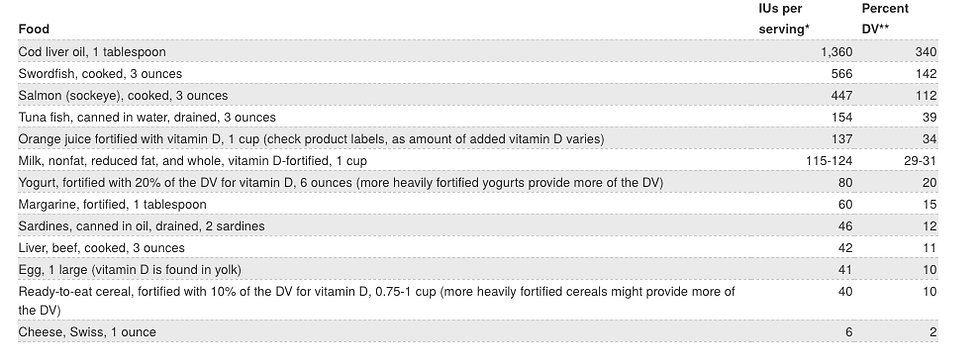
* IUs = International Units. ** DV = Daily Value. The U.S. Food and Drug Administration (FDA) developed DVs to help consumers compare the nutrient contents of products within the context of a total diet. The DV for vitamin D used for the values in Table above is 400 IU for adults and children age 4 years and older. This DV, however, is changing to 20 mcg as the updated Nutrition and Supplement Facts labels are implemented. The updated labels and DVs must appear on food products and dietary supplements beginning in January 2020, but they can be used now. FDA does not currently require food labels to list vitamin D content unless a food has been fortified with this nutrient, but it requires vitamin D content to be listed on the updated labels. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
Sun exposure
Most people meet at least some of their vitamin D needs through exposure to sunlight . Ultraviolet (UV) B radiation with a wavelength of 290–320 nanometers penetrates uncovered skin and converts cutaneous 7-dehydrocholesterol to previtamin D3, which in turn becomes vitamin D3. Season, time of day, length of day, cloud cover, smog, skin melanin content, and sunscreen are among the factors that affect UV radiation exposure and vitamin D synthesis. Perhaps surprisingly, geographic latitude does not consistently predict average serum 25(OH)D levels in a population.
Ample opportunities exist to form vitamin D (and store it in the liver and fat) from exposure to sunlight during the spring, summer, and fall months even in the far north latitudes.
Complete cloud cover reduces UV energy by 50%; shade (including that produced by severe pollution) reduces it by 60%. UVB radiation does not penetrate glass, so exposure to sunshine indoors through a window does not produce vitamin D. Sunscreens with a sun protection factor (SPF) of 8 or more appear to block vitamin D-producing UV rays, although in practice people generally do not apply sufficient amounts, cover all sun-exposed skin, or reapply sunscreen regularly. Therefore, skin likely synthesizes some vitamin D even when it is protected by sunscreen as typically applied.
The factors that affect UV radiation exposure and research to date on the amount of sun exposure needed to maintain adequate vitamin D levels make it difficult to provide general guidelines. It has been suggested by some vitamin D researchers, for example, that approximately 5–30 minutes of sun exposure between 10 AM and 3 PM at least twice a week to the face, arms, legs, or back without sunscreen usually lead to sufficient vitamin D synthesis and that the moderate use of commercial tanning beds that emit 2%–6% UVB radiation is also effective. Individuals with limited sun exposure need to include good sources of vitamin D in their diet or take a supplement to achieve recommended levels of intake.
Despite the importance of the sun for vitamin D synthesis, it is prudent to limit exposure of skin to sunlight and UV radiation from tanning beds . UV radiation is a carcinogen responsible for most of the estimated 1.5 million skin cancers and the 8,000 deaths due to metastatic melanoma that occur annually in the United States. Lifetime cumulative UV damage to skin is also largely responsible for some age-associated dryness and other cosmetic changes. The American Academy of Dermatology advises that photoprotective measures be taken, including the use of sunscreen, whenever one is exposed to the sun.
Assessment of vitamin D requirements cannot address the level of sun exposure because of these public health concerns about skin cancer, and there are no studies to determine whether UVB-induced synthesis of vitamin D can occur without increased risk of skin cancer.
Supplementation
As Vit D is fat soluble, it has to be taken with a fatty acid that can serve as a transport.
It is likely easiest to take Vitamin D with a meal, but you can also pair it with a fat like Fish Oil or a teaspoon of coconut oil.
There is anecdotal reports that it might disrupt sleep if taken later in the evening, so it might be better taken earlier in the day as a precaution.
The recommended daily allowance for Vitamin D as mentioned above is currently set at 400-800IU/day, but this is too low for adults. The safe upper limit in the UK is 4,000IU/day. Research suggests that the true safe upper limit is 10,000IU/day.
For moderate supplementation, a 1,000-2,000IU dose of vitamin D3 is sufficient to meet the needs of most of the population. This is the lowest effective dose range. Higher doses, based on body weight, are in the range of 20-80IU/kg daily.
Vitamin D3 supplementation (cholecalciferol) is recommended over D2 supplementation (ergocalciferol), since D3 is used more effectively in the body.
Coach HB
The above information is taken from the folks at examine.com and US National Institutes Of Health




Comments